Description
Herceptin (Trastuzumab) 600mg
Uses
Trastuzumab is used alone or with other medications to treat certain types of breast cancer. It is also used along with other medications to treat certain types of stomach cancer. The types of cancers trastuzumab is used to treat are tumors that produce more than the normal amount of a certain substance called HER2 protein.This medication is called a monoclonal antibody. It works by attaching to the HER2 cancer cells and blocking them from dividing and growing. It may also destroy the cancer cells or signal the body (immune system) to destroy the cancer cells.
Herceptin is indicated for the treatment of adult patients with HER2 positive metastatic breast cancer (MBC):
– as monotherapy for the treatment of those patients who have received at least two chemotherapy regimens for their metastatic disease. Prior chemotherapy must have included at least an anthracycline and a taxane unless patients are unsuitable for these treatments. Hormone receptor positive patients must also have failed hormonal therapy, unless patients are unsuitable for these treatments.
– in combination with paclitaxel for the treatment of those patients who have not received chemotherapy for their metastatic disease and for whom an anthracycline is not suitable.
– in combination with docetaxel for the treatment of those patients who have not received chemotherapy for their metastatic disease.
– in combination with an aromatase inhibitor for the treatment of postmenopausal patients with hormone-receptor positive MBC, not previously treated with trastuzumab.
Early breast cancer
Herceptin is indicated for the treatment of adult patients with HER2 positive early breast cancer (EBC).
– following surgery, chemotherapy (neoadjuvant or adjuvant) and radiotherapy (if applicable) (see section 5.1).
– following adjuvant chemotherapy with doxorubicin and cyclophosphamide, in combination with paclitaxel or docetaxel.
– in combination with adjuvant chemotherapy consisting of docetaxel and carboplatin.
– in combination with neoadjuvant chemotherapy followed by adjuvant Herceptin therapy, for locally advanced (including inflammatory) disease or tumours > 2 cm in diameter (see sections 4.4 and 5.1).
Herceptin should only be used in patients with metastatic or early breast cancer whose tumours have either HER2 overexpression or HER2 gene amplification as determined by an accurate and validated assay (see sections 4.4 and 5.1).
4.2 Posology and method of administration
HER2 testing is mandatory prior to initiation of therapy (see sections 4.4 and 5.1). Herceptin treatment should only be initiated by a physician experienced in the administration of cytotoxic chemotherapy (see section 4.4), and should be administered by a healthcare professional only.
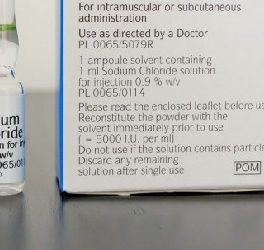
It is important to check the product labels to ensure that the correct formulation (intravenous or subcutaneous fixed dose) is being administered to the patient, as prescribed. Herceptin subcutaneous formulation is not intended for intravenous administration and should be administered via a subcutaneous injection only.
Switching treatment between Herceptin intravenous and Herceptin subcutaneous formulations and vice versa, using the three-weekly (q3w) dosing regimen, was investigated in study MO22982 (see section 4.8).
In order to prevent medication errors it is important to check the vial labels to ensure that the drug being prepared and administered is Herceptin (trastuzumab) and not Kadcyla (trastuzumab emtansine).
Posology
The recommended dose for Herceptin subcutaneous formulation is 600 mg irrespective of the patient’s body weight. No loading dose is required. This dose should be administered subcutaneously over 2-5 minutes every three weeks.
In the pivotal trial (BO22227) Herceptin subcutaneous formulation was administered in the neoadjuvant/adjuvant setting in patients with early breast cancer. The preoperative chemotherapy regimen consisted of docetaxel (75 mg/m²) followed by FEC (5FU, epirubicin and cyclophosphamide) at a standard dose.
See section 5.1 for chemotherapy combination dosing.
Duration of treatment
Patients with MBC should be treated with Herceptin until progression of disease. Patients with EBC should be treated with Herceptin for 1 year or until disease recurrence, whichever occurs first; extending treatment in EBC beyond one year is not recommended (see section 5.1).
Dose reduction
No reductions in the dose of Herceptin were made during clinical trials. Patients may continue therapy during periods of reversible, chemotherapy-induced myelosuppression butthey should be monitored carefully for complications of neutropenia during this time. Refer to the Summary of Product Characteristics (SmPC) for paclitaxel, docetaxel or aromatase inhibitor for information on dose reduction or delays.
If left ventricular ejection fraction (LVEF) percentage drops ≥ 10 points from baseline AND to below 50 %, treatment should be suspended and a repeat LVEF assessment performed within approximately 3 weeks. If LVEF has not improved, or has declined further, or if symptomatic congestive heart failure (CHF) has developed, discontinuation of Herceptin should be strongly considered, unless the benefits for the individual patient are deemed to outweigh the risks. All such patients should be referred for assessment by a cardiologist and followed up.
Missed doses
If the patient misses a dose of Herceptin subcutaneous formulation, it is recommended to administer the next 600 mg dose (i.e. the missed dose) as soon as possible. The interval between consecutive Herceptin subcutaneous formulation administrations should not be less than three weeks.
Special populations
Dedicated pharmacokinetic studies in the elderly and those with renal or hepatic impairment have not been carried out. In a population pharmacokinetic analysis, age and renal impairment were not shown to affect trastuzumab disposition.
Paediatric population
There is no relevant use of Herceptin in the paediatric population.
Method of administration
The 600 mg dose should be administered as a subcutaneous injection only over 2-5 minutes every three weeks. The injection site should be alternated between the left and right thigh. New injections should be given at least 2.5 cm from the old site and never into areas where the skin is red, bruised, tender, or hard. During the treatment course with Herceptin subcutaneous formulation other medicinal products for subcutaneous administration should preferably be injected at different sites. Patients should be observed for six hours after the first injection and for two hours after subsequent injections for signs or symptoms of administration-related reactions (see sections 4.4 and 4.8).
For instructions on use and handling of Herceptin subcutaneous formulation refer to section 6.6.
4.3 Contraindications
• Hypersensitivity to trastuzumab, murine proteins, hyaluronidase or to any of the other excipients listed in section 6.1.
• Severe dyspnoea at rest due to complications of advanced malignancy or requiring supplementary oxygen therapy.
4.4 Special warnings and precautions for use
Traceability
In order to improve the traceability of biological medicinal products, the trade name and the batch number of the administered product should be clearly recorded.
HER2 testing must be performed in a specialised laboratory which can ensure adequate validation of the testing procedures (see section 5.1).
Currently no data from clinical trials are available on re-treatment of patients with previous exposure to Herceptin in the adjuvant setting.
Cardiac dysfunction
General considerations
Patients treated with Herceptin are at increased risk for developing CHF (New York Heart Association [NYHA] Class II-IV) or asymptomatic cardiac dysfunction. These events have been observed in patients receiving Herceptin therapy alone or in combination with paclitaxel or docetaxel, particularly following anthracycline (doxorubicin or epirubicin)–containing chemotherapy. These may be moderate to severe and have been associated with death (see section 4.8). In addition, caution should be exercised in treating patients with increased cardiac risk, e.g. hypertension, documented coronary artery disease, CHF, LVEF of <55%, older age.
All candidates for treatment with Herceptin, but especially those with prior anthracycline and cyclophosphamide exposure, should undergo baseline cardiac assessment including history and physical examination and electrocardiogram (ECG), echocardiogram, and/or multigated acquisition (MUGA) scan or magnetic resonance imaging. Monitoring may help to identify patients who develop cardiac dysfunction. Cardiac assessments, as performed at baseline, should be repeated every 3 months during treatment and every 6 months following discontinuation of treatment until 24 months from the last administration of Herceptin. A careful risk-benefit assessment should be made before deciding to treat with Herceptin.
Trastuzumab may persist in the circulation for up to 7 months after stopping Herceptin treatment based on population pharmacokinetic analysis of all available data (see section 5.2). Patients who receive anthracyclines after stopping Herceptin may possibly be at increased risk of cardiac dysfunction. If possible, physicians should avoid anthracycline-based therapy for up to 7 months after stopping Herceptin. If anthracyclines are used, the patient’s cardiac function should be monitored carefully.
Formal cardiological assessment should be considered in patients in whom there are cardiovascular concerns following baseline screening. In all patients cardiac function should be monitored during treatment (e.g. every 12 weeks). Monitoring may help to identify patients who develop cardiac dysfunction. Patients who develop asymptomatic cardiac dysfunction may benefit from more frequent monitoring (e.g. every 6-8 weeks). If patients have a continued decrease in left ventricular function, but remain asymptomatic, the physician should consider discontinuing therapy if no clinical benefit of Herceptin therapy has been seen.
The safety of continuation or resumption of Herceptin in patients who experience cardiac dysfunction has not been prospectively studied. If LVEF percentage drops ≥ 10 points from baseline AND to below 50%, treatment should be suspended and a repeat LVEF assessment performed within approximately 3 weeks. If LVEF has not improved, or declined further, or symptomatic CHF has developed, discontinuation of Herceptin should be strongly considered, unless the benefits for the individual patient are deemed to outweigh the risks. All such patients should be referred for assessment by a cardiologist and followed up.
If symptomatic cardiac failure develops during Herceptin therapy, it should be treated with standard medicinal products for CHF. Most patients who developed CHF or asymptomatic cardiac dysfunction in pivotal trials improved with standard CHF treatment consisting of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) and a beta-blocker. The majority of patients with cardiac symptoms and evidence of a clinical benefit of Herceptin treatment continued on therapy without additional clinical cardiac events.
Metastatic breast cancer
Herceptin and anthracyclines should not be given concurrently in combination in the MBC setting.
Patients with MBC who have previously received anthracyclines are also at risk of cardiac dysfunction with Herceptin treatment, although the risk is lower than with concurrent use of Herceptin and anthracyclines.
Early breast cancer
For patients with EBC, cardiac assessments, as performed at baseline, should be repeated every 3 months during treatment and every 6 months following discontinuation of treatment until 24 months from the last administration of Herceptin. In patients who receive anthracycline-containing chemotherapy further monitoring is recommended, and should occur yearly up to 5 years from the last administration of Herceptin, or longer if a continuous decrease of LVEF is observed.
Patients with history of myocardial infarction (MI), angina pectoris requiring medical treatment, history of or existing CHF (NYHA Class II –IV), LVEF of < 55%, other cardiomyopathy, cardiac arrhythmia requiring medical treatment, clinically significant cardiac valvular disease, poorly controlled hypertension (hypertension controlled by standard medical treatment eligible), and hemodynamic effective pericardial effusion were excluded from adjuvant and neoadjuvant EBC pivotal trials with Herceptin and therefore treatment cannot be recommended in such patients.
Adjuvant treatment
Herceptin and anthracyclines should not be given concurrently in the adjuvant treatment setting.
In patients with EBC an increase in the incidence of symptomatic and asymptomatic cardiac events was observed when Herceptin (intravenous formulation) was administered after anthracycline-containing chemotherapy compared to administration with a non-anthracycline regimen of docetaxel and carboplatin and was more marked when Herceptin (intravenous formulation) was administered concurrently with taxanes than when administered sequentially to taxanes. Regardless of the regimen used, most symptomatic cardiac events occurred within the first 18 months. In one of the 3 pivotal studies conducted in which a median follow-up of 5.5 years was available (BCIRG006) a continuous increase in the cumulative rate of symptomatic cardiac or LVEF events was observed (up to 2.37 %) in patients who were administered Herceptin concurrently with a taxane following anthracycline therapy, compared to approximately 1 % in the two comparator arms (anthracycline plus cyclophosphamide followed by taxane and taxane, carboplatin and Herceptin).
https://konozahealthbiotech.com
Risk factors for a cardiac event identified in four large adjuvant studies included advanced age (> 50 years), low LVEF (<55%) at baseline, prior to or following the initiation of paclitaxel treatment, decline in LVEF by 10-15 points, and prior or concurrent use of anti-hypertensive medicinal products. In patients receiving Herceptin after completion of adjuvant chemotherapy, the risk of cardiac dysfunction was associated with a higher cumulative dose of anthracycline given prior to initiation of Herceptin and a body mass index (BMI) >25 kg/m2.












Eryn Gerfin –
Terrific article